Background:
Diffuse large B cell lymphoma (DLBCL) constitutes most cases of both primary and secondary central nervous system lymphoma (CNSL). They represent a highly aggressive subset of non-Hodgkin lymphoma and prognosis varies depending on the cell of origin. Immunohistochemistry using antibodies for CD10, BCL-6, and MUM-1, also known as the Hans algorithm, is the most common method for determining the cell of origin and predicting outcomes in DLBCL. The study by Hans et al. found that the germinal center B-cell-like (GCB) group had a much better prognosis compared to the non-GCB group, with 5-year overall survival (OS) of 76% and 34% respectively. Despite chemotherapy, recurrence is common in these patients, and up to 40-50% do not achieve durable remission. It is important to identify who may benefit from more aggressive or experimental therapy at diagnosis. Stereotactic radiosurgery (SRS) is the administration of a localized, high dose of ionizing radiation and limited studies exist exploring SRS as a treatment modality in relapsed/refractory (r/r) CNSL or prognostic implications of the Hans algorithm in these patients.
Aim/Objective:
To perform a retrospective analysis of outcomes of patients with CNSL, phenotypes determined by the Hans algorithm, treated with SRS at a single comprehensive cancer center.
Methods:
We studied the demographic, clinical, pathological, and treatment characteristics of r/r CNSL patients (N=27), age ≥ 18 years, who received SRS at Roswell Park Comprehensive Cancer Center between 01/2000 and 01/2023. The Hans algorithm was used to group the patients into non-GCB (N=17) and GCB (N=10) cohorts. Overall survival (OS) and progression-free survival (PFS) were calculated and reported using Kaplan-Meier analyses and log-rank tests. Cox regression models were used to describe cross-cohort comparisons of survival.
Results:
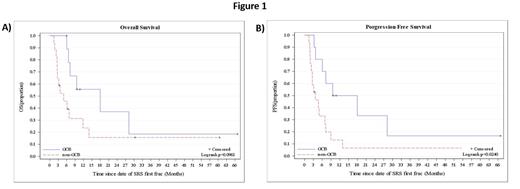
The median Karnofsky performance status at diagnosis was 70 for both groups. The overall response rate (ORR) to SRS in GCB-type was 80% (7 complete response and 1 partial response; CR, PR). The ORR in non-GCB type was 58% (6 CR and 4 PR). Post-SRS, stem cell transplant (SCT) was avoided in 100% of the patients in the GCB group, while 17% of the patients in the non-GCB group received SCT. The 6-month overall survival (OS) rate was 100% and 46% for the GCB-type and non-GCB type respectively (p=0.096, Figure 1A). The 6-month progression-free survival (PFS) rate was 80% for the GCB-type and 33% for the non-GCB type (p=0.024, Figure 1B). In the GCB group, the median OS was 18.0 months while the median PFS was 13.8 months. In the non-GCB group, the median OS was 4.9 months while the median PFS was 3.6 months. The median time from chemotherapy completion to SRS administration was 8.0 months in the GCB-type and 2.0 months in the non-GCB type.
Conclusion:
Our data support that the GCB-type predicts a more favorable outcome in CNSL, with improved OS and PFS rates compared to the non-GCB type. In addition, the non-GCB type patients required earlier SRS administration and had a lower ORR to SRS. Classifying CNSL into GCB and non-GCB phenotypes using the Hans algorithm might help characterize patients into groups with different prognoses.
Disclosures
Hernandez-Ilizaliturri:Dava Oncology: Consultancy; AbbVie: Consultancy; Amgen: Consultancy; Epizyme: Consultancy; Novartis: Consultancy; BMS: Consultancy; Incyte/Morphosys: Consultancy; BioGene: Consultancy; Collectar: Consultancy; Gilead: Consultancy; Kite: Consultancy; ADC Therapeutics: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal